 The cleft lip is usually repaired when a child is 2-3 months old; depending on your child's size and their overall health. This surgery repairs the gap in the lip that extends into the nose and includes the skin, the muscle of the mouth and the mucosa on the inside of the lip. The flattening of the nose on the side of the cleft is repaired at same time the lip is repaired.
The cleft lip is usually repaired when a child is 2-3 months old; depending on your child's size and their overall health. This surgery repairs the gap in the lip that extends into the nose and includes the skin, the muscle of the mouth and the mucosa on the inside of the lip. The flattening of the nose on the side of the cleft is repaired at same time the lip is repaired.
There are a number of techniques for repairing the cleft lip. The surgery is tailored to your child's cleft. The procedure is slightly different if your child has a bilateral cleft lip (cleft going into both nostrils) or a unilateral cleft lip (cleft going into one nostril).
Unilateral Cleft Lip Repair
Children with a unilateral cleft lip (a gap in the lip going into one nostril) need a surgery to rotate the central side of the lip down. There is less tissue and this elongates the shorter central side of the cleft lip. The lateral (outside) of the cleft lip is advanced across the defect. The muscle is brought together to recreate the circle of muscle around the mouth.
There are many ways of accomplishing this. Dr. Skirko hides the scars in the subtle natural lines of the lip and nose so that is mirrors the non-cleft side. This camouflages the scar in natural lines. Most older techniques have scars that cross the midline and violate the central lip (philtral column). Scars here draw your attention more. Some have incisions in areas that causes problematic scarring. Dr. Skirko uses a newer technique was developed to follow the natural lines and hides the scars in these naturally occurring contours. This technique is called the anatomic subunit technique. While there is no 'Gold Standard,' having a surgeon comfortable with several techniques will allow them to tailor the repair to your child's lip defect.
What Sets Us Apart?
The principles of reconstruction on the face often utilize hiding scars in natural contours to improve the final result. Our surgeons are well versed in these techniques and can often utilize cleft lip repair that is based on these natural contours. While the long-term results comparing these newer techniques to older 'cut as you go' techniques haven't yet been reported, families and teams using these newer techniques are often very pleased with the result at the lip and just inside the nose. This repair can only be performed on children with a unilateral cleft. Your surgeon can discuss the specifics of your child's repair during your visit.
Our surgeons have extensive training and experience in cleft lip repair as well as the removal of masses from the lips. Our surgeons focus their work on children with conditions of the face, head and neck. This provides us with unique training and experiences. Not only are we experts in making the face, nose and throat look normal, but we are also experts in helping optimize the function of these critical areas.
In addition to extensive training, our surgeons are often asked to repair lip scars. Performing these lip scar revisions has helped us have a deep understanding of the subtleties in primary cleft lip repair to avoid these scarring problems. With these experiences, we continue to refine portions of cleft lip repair to optimize your child's outcome.
Bilateral Cleft Lip Repair
For a bilateral cleft lip, the lip skin in the center of your child's face does not have muscle. The muscle from the two sides is stretched across under the central skin. The skin on the central lip will make up the center of your child's new lip. The bone behind the central lip (where your child's front teeth will come in later) is sometimes pushed out too far. Nasolabial molding is helpful in pulling this bone back into position and making the lip repair more successful. Part of the lip repair involves reshaping the nose, both the way it looks on the outside as well as just inside the nose and how the nose works.
What Sets Us Apart?
Our surgeons have extensive training and experience in cleft lip repair as well as the removal of masses from the lips. Our surgeons focus their work on children with conditions of the face, head and neck. This provides us with unique training and experiences. Not only are we experts in making the face, nose and throat look normal, but we are also experts in helping optimize the function of these critical areas.
Families often seek our help in repairing their child's lip scars. Performing these lip scar revisions helps us have a deep understanding of the subtleties in primary cleft lip repair to avoid these scarring problems. We continue to refine portions of cleft lip repair to optimize your child's outcome.
Primary Cleft Rhinoplasty
Infants with a cleft lip and varying degrees of abnormality with the way their nose looks. Often the cartilage that keeps the nose 'springing open' is slightly smaller than normal, is often positioned abnormally, and is often flattened. Addressing only the cleft in the lip will leave your child with asymmetry of nose until it is surgically repaired. The repair of the cleft lip can allow your surgeon access to the nasal space. Using minimally invasive techniques through the lip incisions, your surgeon will reposition the nasal cartilage in a more normal position. The skin and cartilage are usually held in their new position with sutures that may be seen on the side your child’s nose. Sutures often are needed on the side of the nose as well. The suture will either be dissolvable or will have a small piece of gauze 'bolster.' The amount of repair required for the nose depends on the deformity.
What Sets Us Apart?
Infants have to breathe through their nose and disorders affecting the nasal airway are serious in babies. For example, an infant will breathe through their nose and eat through their mouth at the same time. Sometimes these disorders are less serious but don't allow a baby to feed easily. Other infants have growths inside of their nose and sinuses that need to be removed and depending on the growth may need reconstruction
Our surgeons diagnose and manage these problems regularly. We have an in-depth understanding of nasal anatomy and the function of the nasal passages. We utilize this experience at the time of the initial repair, but also as children grow and develop problems with the inside or outside of their nose.
Tailored Care
Some children need additional small modification of their nasal procedure to optimize their nose. Sometimes this involves limited repositioning of the septum. Sometimes this involved different techniques to stabilize the nasal cartilage in a normal position. Your surgeon will assess your child's cleft and review the plan with you so that any questions you have can be answered.
What To Expect
- When you meet your surgeon to discuss surgery, you will receive a handout that details what to expect as well as home care your child will need. Reviewing this before surgery with your surgeon and our clinic nurses will make the time after surgery less stressful.
- For a week or two after surgery, your child will likely need a little extra care and attention. You shouldn't be concerned about 'spoiling' your child while they are recovering. It is ok to help your child through their recovery with extra holding and comforting.
- Children stay in the hospital one or two nights depending on how well they recover from surgery.
- Your child will have an IV that will be used to give your child fluids (to keep them hydrated) and IV pain meds if the pain medications they take by mouth aren't enough.
- They may have small flexible stents in their nose to help with healing.
- Your child's lip and nose will likely be swollen.
- Most if not all of the sutures will be dissolvable. In certain circumstances, your surgeon may feel sutures that need to be removed will be a better result. These sutures are usually removed in clinic.
- Your child will receive pain medication and this will be adjusted to ensure their pain is well controlled.
- Your child will be closely monitored for pain control, breathing and how much they are eating/drinking.
- Your child will usually wear 'Arm Straighteners' that help prevent them from accidently hurting themselves while they are healing
Common Questions
How will I feel about how my child looks after surgery?
After surgery, your child will look different. This is often very emotional time. Some parents miss the 'big smile' of their child with a cleft, but they are excited to see their child's new face. The nurses and staff at Diamond Children's will help you through this exciting time.
Are there restriction on how my child can eat?
Our surgeons don't put restrictions on how you child eats or drinks. Your child can use whatever bottle or cup they used before surgery. Problems with healing are very uncommon and these restrictions don't seem to decrease the likelihood of having a problem. Most children are able to drink and eat soon after surgery, but some kids refuse. Your nurse will work to figure out what your child needs to help them eat.
Will my child be able to drink after the cleft lip surgery?
Most children do well eating and drinking after cleft lip surgery. Their lip and face is soar but it is uncommon to have enough pain to prevent them from drinking. Sometimes babies need stronger pain medications to make them comfortable. We will monitor your baby closely to ensure they have the pain medications they need.
If your child needs stronger pain medications, they might get constipated. If this happens, usually a couple ounces of apple or pear juice helps to get things moving. Check with your surgeon to make sure this is ok for your baby.
Do I need to clean out the nasal stents if my surgeon chooses to use them?
Infants have to breathe through their noses. If the nose stents become clogged, they may have trouble breathing and eating. Infants breath faster than we do, so they need to coordinate breathing and eating. If they are having trouble breathing, difficulties with feeding is sometimes one of the first things we notice. Sometimes fixing this is as simple as putting saline (salt water) drops in the nose. If your child's stents are starting to clog, you can use saline with every diaper change to thin the secretion. Other times the stents need to be replaced or cleaned out. If your baby is having trouble breathing, you should call your provider.
We are starting to use newer nasal stents that stay in on their own and can be removed for cleaning at home. Your surgeon can discuss whether these are right for your child.

 Cleft Lip & Palate
Cleft Lip & Palate

 Parents that learn their child has a cleft lip and or palate during pregnancy can have many questions and our team can help get you ready to care for your child with a cleft. Ultrasounds are more able to diagnose cleft lip prior to delivery and can identify an isolated cleft palate to some degree as well. Prenatal counseling is an option we offer families to help them understand cleft lip and palate and answer all the questions they have. It is often helpful in taking the mystery out of the problem.
Parents that learn their child has a cleft lip and or palate during pregnancy can have many questions and our team can help get you ready to care for your child with a cleft. Ultrasounds are more able to diagnose cleft lip prior to delivery and can identify an isolated cleft palate to some degree as well. Prenatal counseling is an option we offer families to help them understand cleft lip and palate and answer all the questions they have. It is often helpful in taking the mystery out of the problem. Feeding and Weight Gain
Feeding and Weight Gain Nasolabial Molding
Nasolabial Molding The cleft lip is usually repaired when a child is 2-3 months old; depending on your child's size and their overall health. This surgery repairs the gap in the lip that extends into the nose and includes the skin, the muscle of the mouth and the mucosa on the inside of the lip. The flattening of the nose on the side of the cleft is repaired at same time the lip is repaired.
The cleft lip is usually repaired when a child is 2-3 months old; depending on your child's size and their overall health. This surgery repairs the gap in the lip that extends into the nose and includes the skin, the muscle of the mouth and the mucosa on the inside of the lip. The flattening of the nose on the side of the cleft is repaired at same time the lip is repaired.  The cleft in the lip often extending into the gum and the palate. If the cleft extends into the palate, it needs to be repaired with a surgery that brings the tissue together and realigns the soft palate muscles. The procedure is slightly different in children with a cleft of the palate without a cleft lip.
The cleft in the lip often extending into the gum and the palate. If the cleft extends into the palate, it needs to be repaired with a surgery that brings the tissue together and realigns the soft palate muscles. The procedure is slightly different in children with a cleft of the palate without a cleft lip. 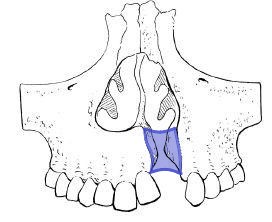 The cleft in the lip often extending into the gum and the palate. If the cleft extends into the palate, it needs to be repaired with a surgery that brings the tissue together and realigns the soft palate muscles. The procedure is slightly different in children with a cleft of the palate without a cleft lip.
The cleft in the lip often extending into the gum and the palate. If the cleft extends into the palate, it needs to be repaired with a surgery that brings the tissue together and realigns the soft palate muscles. The procedure is slightly different in children with a cleft of the palate without a cleft lip.