 Velopharyngeal Insufficiency (VPI) is a problem where the soft palate does not close off the nose from the mouth. This results in air escaping through the nose while talking and sometimes liquids escaping through the nose while drinking. Children with a history of a cleft palate (with or without a cleft lip) are at risk of developing this problem. Other children can also have this problem as well.
Velopharyngeal Insufficiency (VPI) is a problem where the soft palate does not close off the nose from the mouth. This results in air escaping through the nose while talking and sometimes liquids escaping through the nose while drinking. Children with a history of a cleft palate (with or without a cleft lip) are at risk of developing this problem. Other children can also have this problem as well.
VPI is usually diagnosed by a speech and language pathologist analyzing the way your child's voice sounds with difference phrases and in conversational speech. This assessment is called perceptual speech analysis. Speech and language pathologists also may perform a test comparing the amount of air that escapes from the mouth and nose during speech (called naso-metry). When there is concern for some degree of VPI, we often need to understand the anatomy at the back of the nose/throat to help guide treatments (see below for details about this part of the exam)
VPI and Quality of Life
In addition to making it hard to understand what your child is saying, having VPI can have a negative impact on your child's life. Another term for this "impact" is quality of life. One of our surgeons, Dr. Skirko, has done extensive research on the impact VPI has on quality of life. Part of this work developed and tested a new VPI specific quality of life instrument. This instrument is now being translated to several other languages and is being used by cleft teams around the globe.
While these are important milestones for VPI research, Dr. Skirko's studies also highlight two problems that are often overlooked in managing children with VPI:
1) Children with 'mild' VPI can have severely impacted quality of life.
Even children with more 'mild' categories of VPI can have a low (or worse) quality of life than children without VPI and treatment improves nearly always improves their quality of life. Depending on these children's flexible exam, these children often can have a large improvement in their quality of life with surgery for VPI.
2) Parents of older children often don't understand the full impact VPI has on their child's life.
While parents of children with VPI usually know if their child is having problems or not, the degree of trouble they are having is often underestimated by parents. When parents and children both complete the questionnaire, there is often a difference between a child's response and their parents. Reviewing both parent and child's responses help to identify areas that children haven't fully shared with their parents. This can be very helpful in understanding the problems our surgeons are going to try improving with treatment, usually surgery.
 The 'Scope' Exam
The 'Scope' Exam
To see the area behind the palate (the velum), a small flexible telescope is inserted through the nose. Most kids tolerate this very well after getting used to the funny feeling. With the camera in position, your child will then say some specific phrases with the speech and language pathologist listening and helping. The way throat closes behind the palate while your child is talking will help guide the treatment your surgeon's plans. We perform this endoscopic exam many times per day on children to help understand problems in the nose, throat and voice box.
Treatment of VPI
Occasionally, Children with VPI need treatment for their hypernasality (VPI) but are not a candidate for surgery. While this is uncommon, it can include severe airway obstruction, progressive disease causing the VPI or medical problems that reduces the advisability of surgery. These children are often treated with a prosthetic. This is a device that is clasped to the teeth and the back of the device blocks air from escaping through the nose. The device can be removed at night, so it can be helpful in children with airway obstruction/sleep apnea.
Most children with VPI require surgery to correct the problem leading to VPI. There are several surgeries that are used to treat VPI and the decision for which surgery is the best option for your child will depend on how their palate moves and the way the back of the nose/throat looks. Your pediatric facial plastic surgeons and speech pathologist will review all the information (including the flexible exam) to develop the best plan for your child.
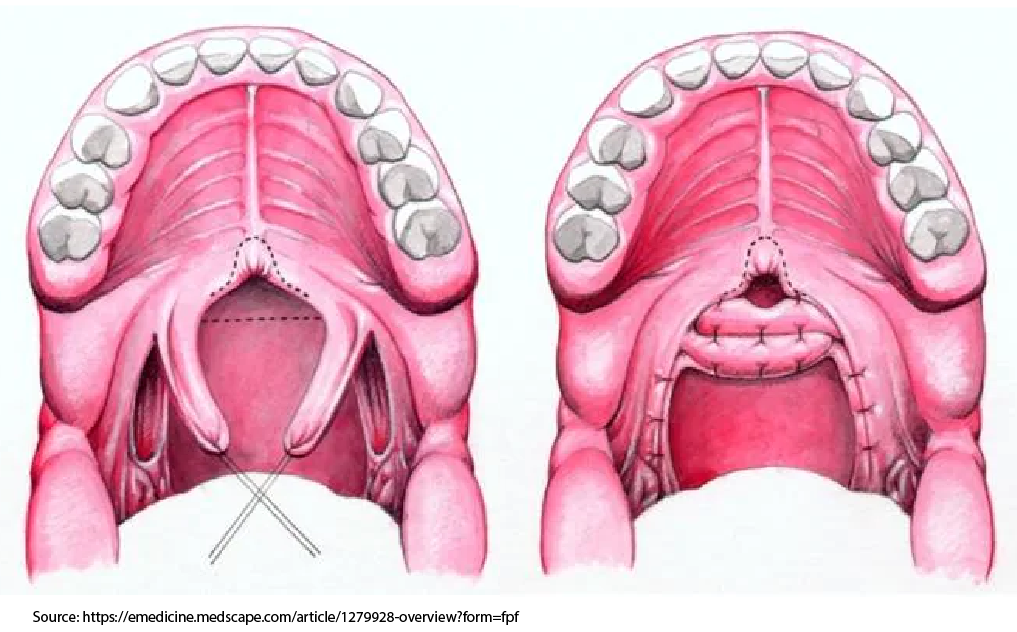
Furlow Palatoplasty for VPI
If your child has a persistent abnormality of the muscles in the palate, a surgery to lengthen the palate and re-align the muscles in the palate may be needed. This surgery is similar to the surgery used to close the soft palate in children with a cleft of the soft palate alone. This surgery lengthens the soft palate and moves the muscles so that they are running across the palate (the normal orientation) rather than running front to back (the orientation in children with a cleft palate). The decision to perform this surgery alone usually depends on the size of the gap and the orientation of the muscles.
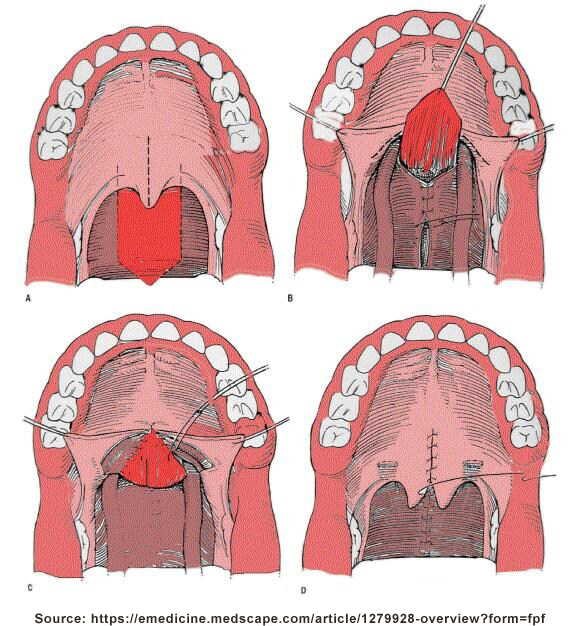
 Sphincter Pharyngoplasty for VPI
Sphincter Pharyngoplasty for VPI
Some children have a palate with muscles that have been moved to the correct orientation, but still have a palate that is too short to reach the back of the throat. Depending on the size and shape of the gap, many of these children have significant improvement with a surgery to create a "speed bump" at the back of the throat. This procedure called a Sphincter Pharyngoplasty takes a piece of tissue that runs behind the tonsil and moves it to run across the throat behind the palate. Usually there is one on each side except for rare problems. These pieces of tissue are often called a 'flap' by your surgeons. If the flaps are too big, sit too low or end in the wrong location, they can cause problems. These problems range from not being able to breathe very well through your child's nose (uncommon) to scarring that blocks off the space between the nose and throat (rare). While it is uncommon, your child can also develop sleep apnea after the procedure.
Tailored Care
Nearly every Sphincter Pharyngoplasty is customized to fit your child's gap. From the size of the flaps, to the position on the side of the throat, to the height of placement of the flaps. Customizing the procedure to treat your child's VPI but not over doing it helps to minimize the risk of sleep apnea.
 Pharyngeal Flap for VPI
Pharyngeal Flap for VPI
Some children with VPI have a large gap or a palate that does not move enough to make a sphincter a viable option. For these children, a pharyngeal flap is usually the best surgical option. In this procedure, a piece of tissue from the back for the throat is connected to the back of the soft palate. This blocks the air escaping through the nose but allows your child to breathe through their nose.
Tailored Care
This flap is often customized and minor adjustments are made to treat your child's VPI but minimize the risk of sleep apnea and scaring.
What Sets Us Apart?
Our surgeons focus their work on children with conditions of the face, head, throat and neck. This provides us with unique training and experiences. We have also developed tools to help other surgeons and cleft team measure VPI outcomes in a new way. By asking children and families how much of a problem they are having. Some surgeons forget the reason we are operating is to improve your child's daily interactions. While tests of nasal emission are sometimes helpful, our VPI quality of life instrument (the VELO) measures the very thing we are trying to improve. Quality of Life.
We are passionate about helping your child as well as helping surgeons around the globe provide better care to children just like yours.



 Velopharyngeal Insufficiency (VPI) is a problem where the soft palate does not close off the nose from the mouth. This results in air escaping through the nose while talking and sometimes liquids escaping through the nose while drinking. Children with a history of a cleft palate (with or without a cleft lip) are at risk of developing this problem. Other children can also have this problem as well.
Velopharyngeal Insufficiency (VPI) is a problem where the soft palate does not close off the nose from the mouth. This results in air escaping through the nose while talking and sometimes liquids escaping through the nose while drinking. Children with a history of a cleft palate (with or without a cleft lip) are at risk of developing this problem. Other children can also have this problem as well. The 'Scope' Exam
The 'Scope' Exam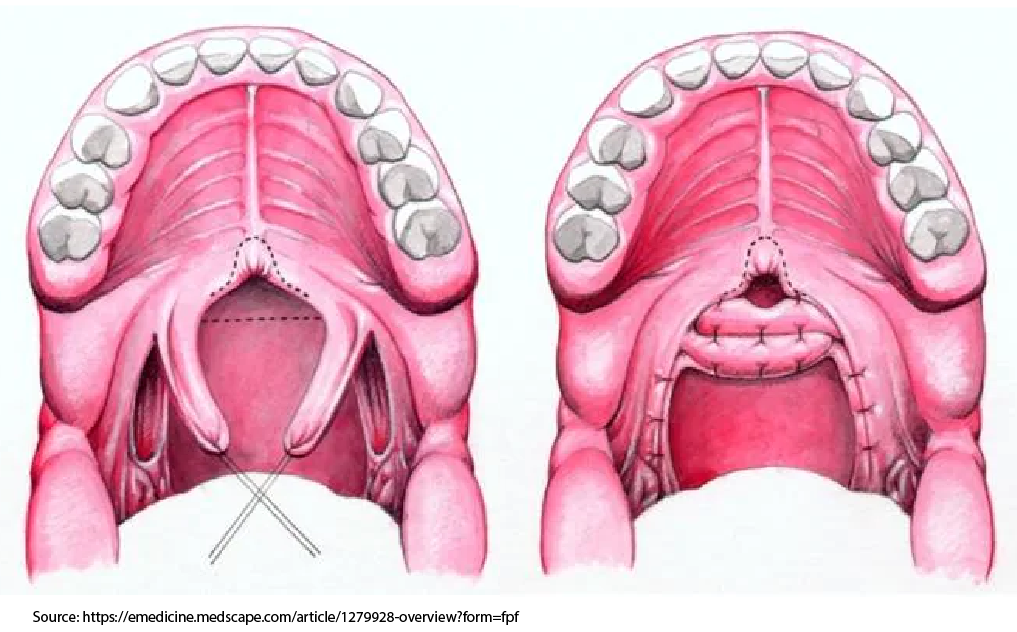 Sphincter Pharyngoplasty for VPI
Sphincter Pharyngoplasty for VPI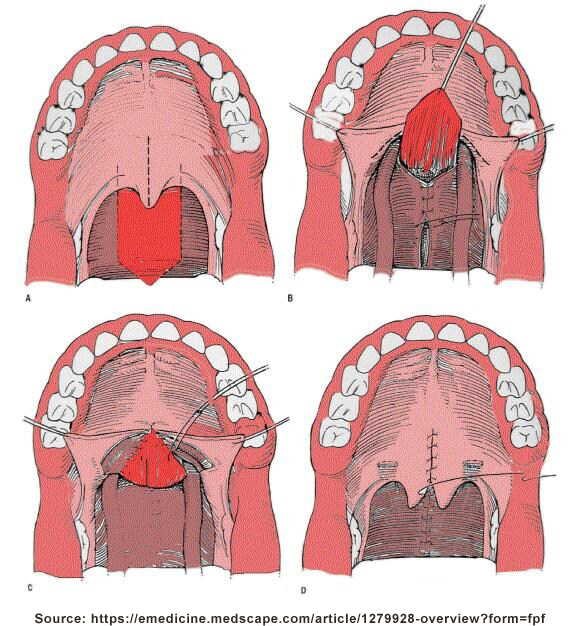 Pharyngeal Flap for VPI
Pharyngeal Flap for VPI Orthodontics and dental care are important to optimize outcomes in children with cleft lip and palate. Children with clefts have typical dental needs as well as special problems that are unique to cleft care. Dental hygiene is important as unhealthy teeth and gums compromise future orthodontic and surgery of the jaws. It also contributes to low self-esteem and psychosocial issues. The orthodontist will help monitor facial growth positioning bony segments to provide the underlying framework for the facial soft tissue. If the bone of the face and teeth are not in the correct place, the facial appearance will suffer.
Orthodontics and dental care are important to optimize outcomes in children with cleft lip and palate. Children with clefts have typical dental needs as well as special problems that are unique to cleft care. Dental hygiene is important as unhealthy teeth and gums compromise future orthodontic and surgery of the jaws. It also contributes to low self-esteem and psychosocial issues. The orthodontist will help monitor facial growth positioning bony segments to provide the underlying framework for the facial soft tissue. If the bone of the face and teeth are not in the correct place, the facial appearance will suffer.  Children with a cleft lip and palate often also have difficulty with a sunken in face (midface) around the nose (maxillary hypoplasia). This usually results in a hollow appearance of their face but also causes dental and chewing problems because the teeth don't line up properly. If your child has this problem, they will eventually need a surgery where the bones in the central face and upper jaw are moved forward. This is called a LeFort 1 osteotomy (cutting the bone of the midface) and maxillary advancement (bringing the midface forward). This can be done slowly or all at once. If a child has a severe sunken in midface, they may require this in grade school (usually between the ages of 6 and 9). Slowly moving the upper jaw bone involves distraction osteogenesis. For this procedure the upper jaw is cut and then after a 'bone scar' forms, the upper jaw is slowly advanced to its final position. The midface is slowly pulled forward in one of two ways. Sometimes we are able to place devices in the tissue with a flexible arm (or activator) sitting in the upper gum line that allows us to advance the device slowly. Sometimes we need to use a type of 'headgear' that is more stable (HALO device). The force of slowly moving the upper jaw forward stimulates bone growth at the 'bone scar.' After the upper jaw is in the desired position, the bone continues to harden over several weeks.
Children with a cleft lip and palate often also have difficulty with a sunken in face (midface) around the nose (maxillary hypoplasia). This usually results in a hollow appearance of their face but also causes dental and chewing problems because the teeth don't line up properly. If your child has this problem, they will eventually need a surgery where the bones in the central face and upper jaw are moved forward. This is called a LeFort 1 osteotomy (cutting the bone of the midface) and maxillary advancement (bringing the midface forward). This can be done slowly or all at once. If a child has a severe sunken in midface, they may require this in grade school (usually between the ages of 6 and 9). Slowly moving the upper jaw bone involves distraction osteogenesis. For this procedure the upper jaw is cut and then after a 'bone scar' forms, the upper jaw is slowly advanced to its final position. The midface is slowly pulled forward in one of two ways. Sometimes we are able to place devices in the tissue with a flexible arm (or activator) sitting in the upper gum line that allows us to advance the device slowly. Sometimes we need to use a type of 'headgear' that is more stable (HALO device). The force of slowly moving the upper jaw forward stimulates bone growth at the 'bone scar.' After the upper jaw is in the desired position, the bone continues to harden over several weeks.  Children with a cleft lip and palate often have a nose that doesn't look like other kids. Even if the outside appearance of the nose is normal, the inside of the nose tends to be twisted. Rhinoplasty (or a 'nose job') is a nasal reconstruction to improves the appearance of the nose as well as a child's ability to breathe through their nose. Ideally, we wait until a patient's face reaches their adult size to perform definitive (final) nasal surgery. The reason we try to wait is due to concern that the nose will not grow as well if we operate earlier. Studies that have carefully evaluated this possibility have not shown a clear answer.
Children with a cleft lip and palate often have a nose that doesn't look like other kids. Even if the outside appearance of the nose is normal, the inside of the nose tends to be twisted. Rhinoplasty (or a 'nose job') is a nasal reconstruction to improves the appearance of the nose as well as a child's ability to breathe through their nose. Ideally, we wait until a patient's face reaches their adult size to perform definitive (final) nasal surgery. The reason we try to wait is due to concern that the nose will not grow as well if we operate earlier. Studies that have carefully evaluated this possibility have not shown a clear answer.  Unfortunately, sometimes a well repaired cleft lip scars in an unfavorable way. Each cleft scar is a little different than the rest. When to address a cleft scar depends on how it is impacting your child. Children can be quick to point out differences and so we often try to improve the scar before a child starts school to help minimize any 'teasing' they may experience. Improving the appearance of the lip in early childhood can be an important step in ensuring your child has confidence in themselves.
Unfortunately, sometimes a well repaired cleft lip scars in an unfavorable way. Each cleft scar is a little different than the rest. When to address a cleft scar depends on how it is impacting your child. Children can be quick to point out differences and so we often try to improve the scar before a child starts school to help minimize any 'teasing' they may experience. Improving the appearance of the lip in early childhood can be an important step in ensuring your child has confidence in themselves. 